By Eric Stann
Feb. 27, 2024
Contact: Eric Stann, 573-882-3346, StannE@missouri.edu
Photos by Abbie Lankitus and Sam O’Keefe
Ground-breaking innovation at the University of Missouri provides patients around the world with access to a lifesaving toolbox of vital pharmaceutical ingredients called radioisotopes produced at only one location in the United States — the University of Missouri Research Reactor (MURR).
Building off more than a half-century of momentum since MURR opened, two MU researchers, Carolyn Anderson and Heather Hennkens, are now leading the way to uncover the benefits of a promising new addition to the toolbox: a radioisotope known as terbium-161.
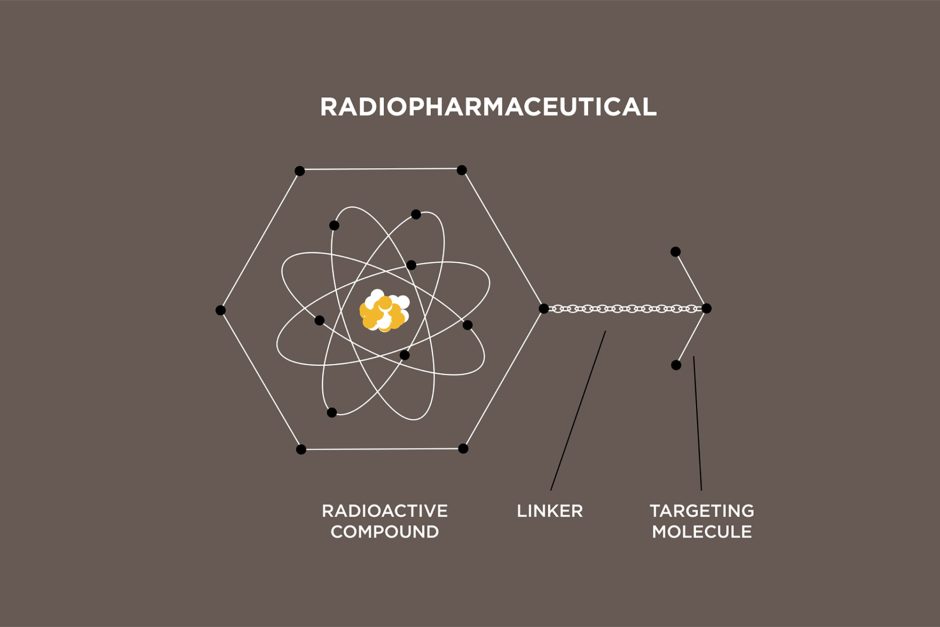
Radiopharmaceuticals contain a small amount of radioactive material. This radioactive “payload” is delivered to specific cancer cells by a “targeting molecule.” The result is a lethal blow to cancer cells.
“By delivering radioisotopes to the site of cancer cells, we can deposit a whole bunch of energy right where these cells are growing and cause DNA double-strand breaks,” said Anderson, director of MU’s Molecular Imaging and Theranostics Center (MITC) and the Simón-Ellebracht Professor in Medicinal Chemistry. “DNA is responsible for allowing cancer cells to multiply, and so if you break that, it will essentially kill the cells or stop them from multiplying.”
Finding the right fit
To determine the right pairing of radioisotope and targeting molecule to maximize the effectiveness of terbium-161, Anderson and Hennkens are focused on different aspects of taking laboratory results into the clinic.
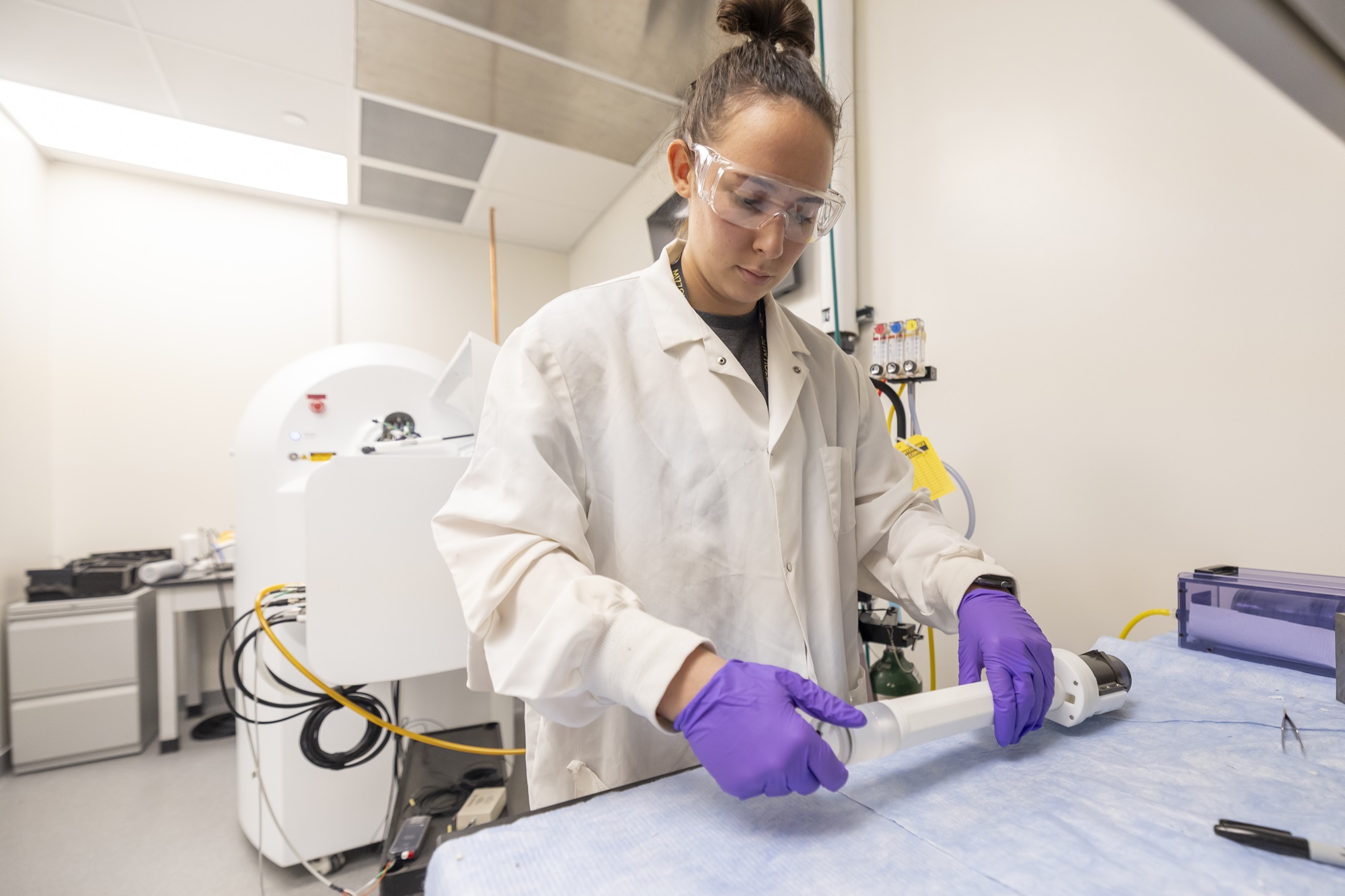
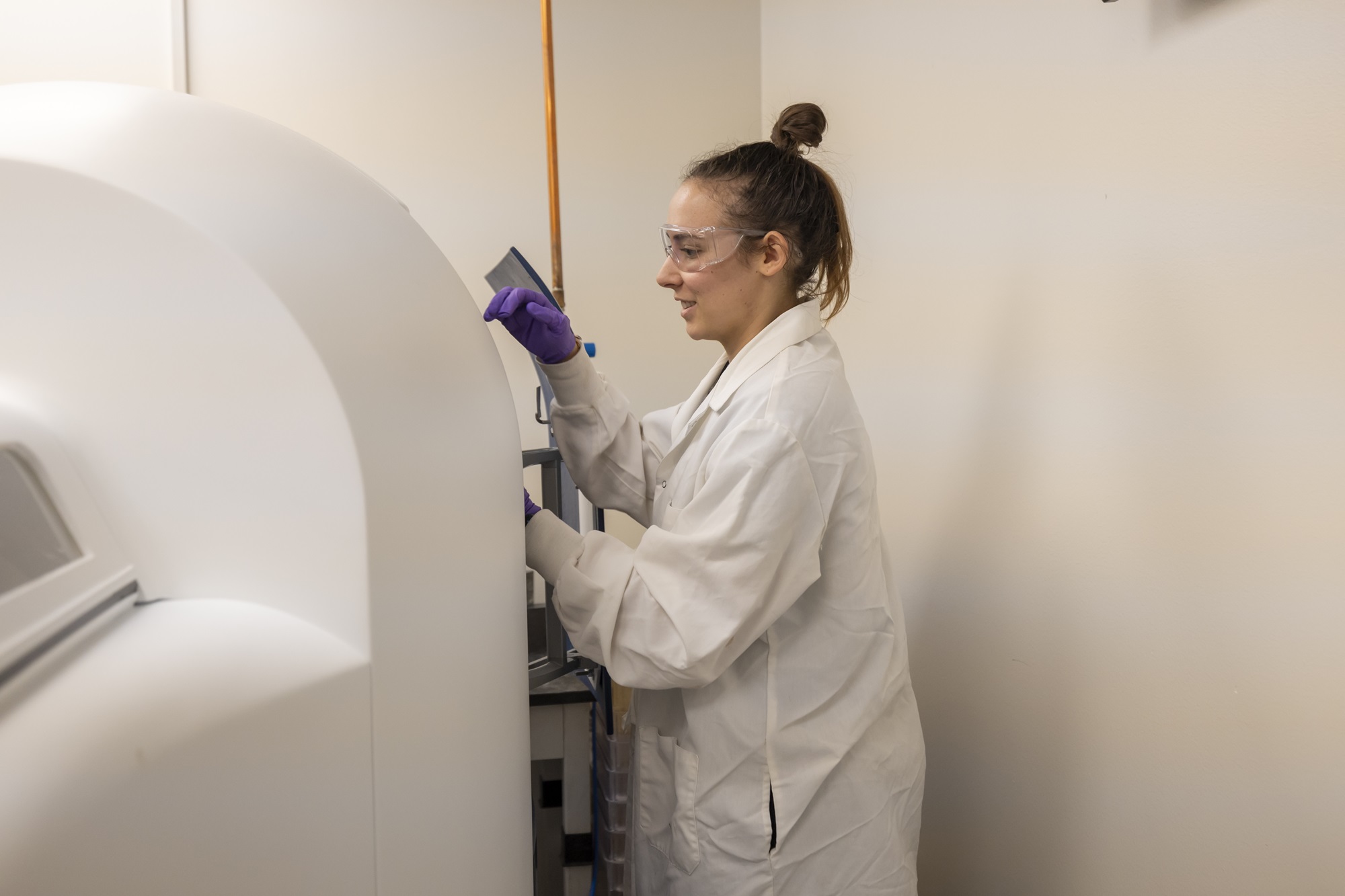
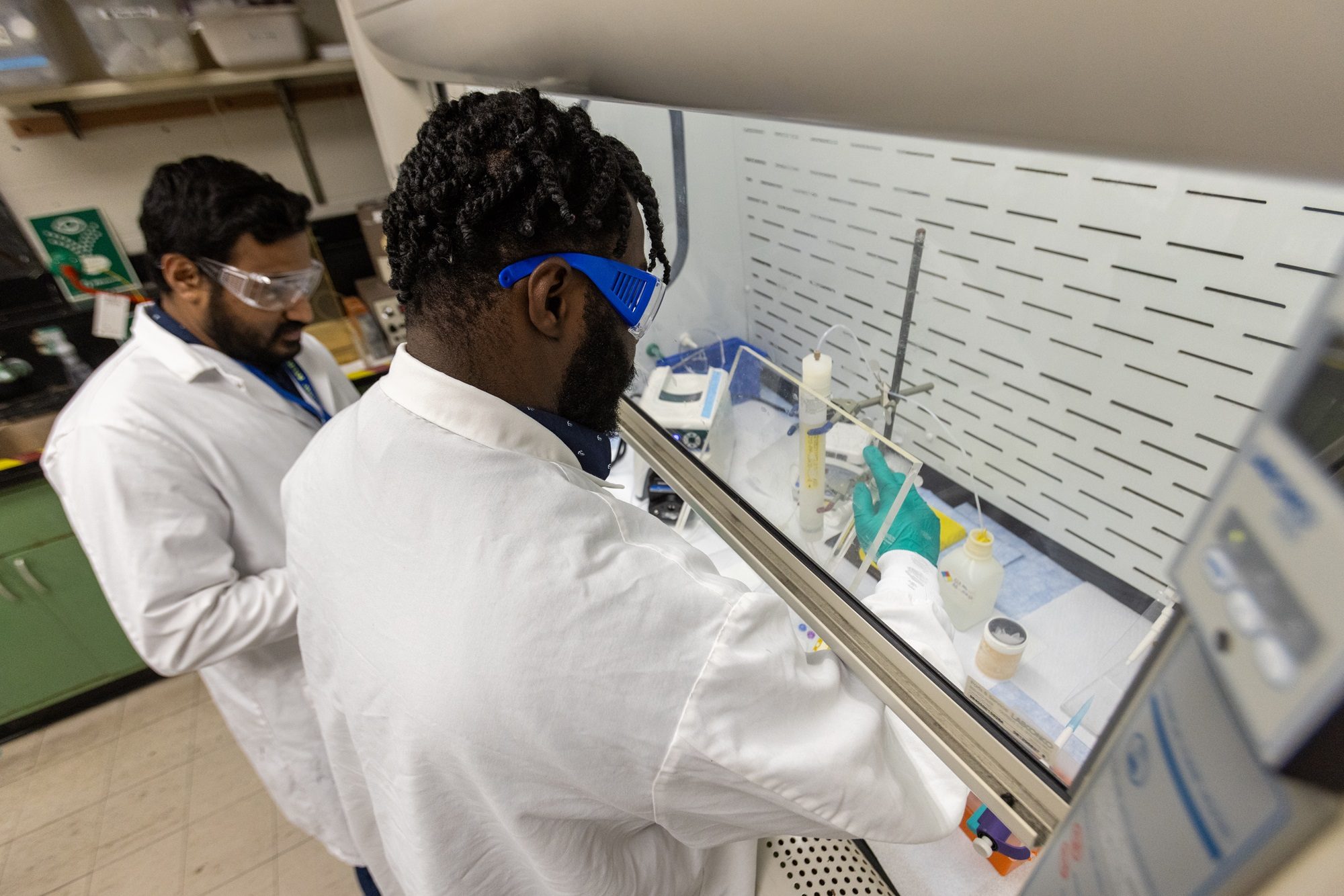
Hennkens’ team is working on producing the “payload” or radioactive isotope to be delivered to a tumor cell. She said the process requires purifying and formulating the radioisotope to make sure it can be effectively incorporated into the radiopharmaceutical.
“One exciting aspect of terbium-161 is its emission of an abundance of low-energy electrons, which are released in addition to electrons with moderate energy that are similar to those of existing clinical radiopharmaceuticals,” said Hennkens, an assistant professor in the MU Department of Chemistry. “As terbium-161 decays, these low-energy electrons can deposit a large amount of energy in a small area, which creates a lot of damaging power. Therefore, with the right placement, we could potentially see increased therapeutic efficacy with this radioisotope.”
The right placement is critical for stopping the spread of cancer, said Anderson, who has known Hennkens since their days at Washington University in St. Louis more than 20 years ago when Hennkens was a graduate student and Anderson was a faculty member.
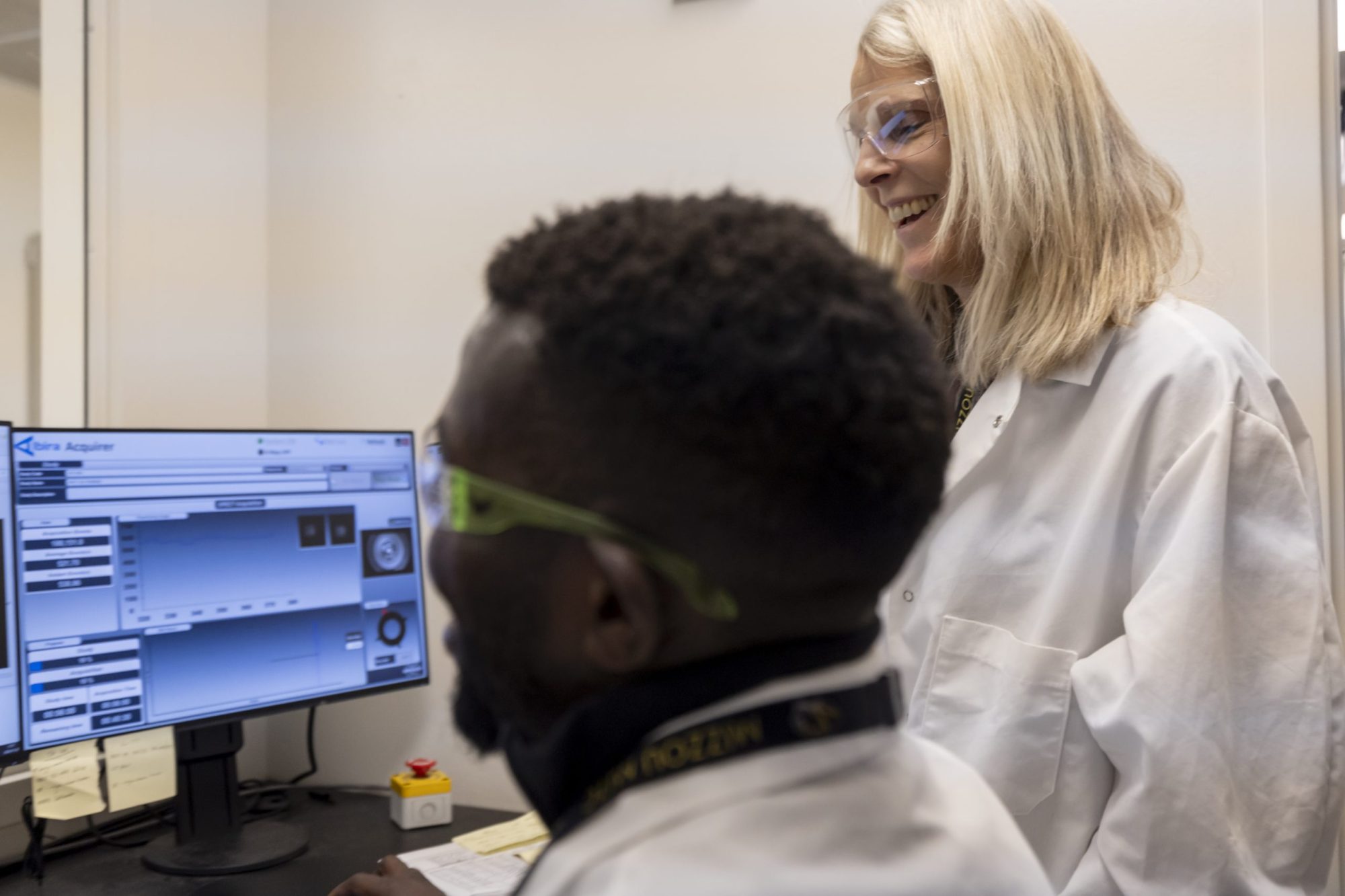
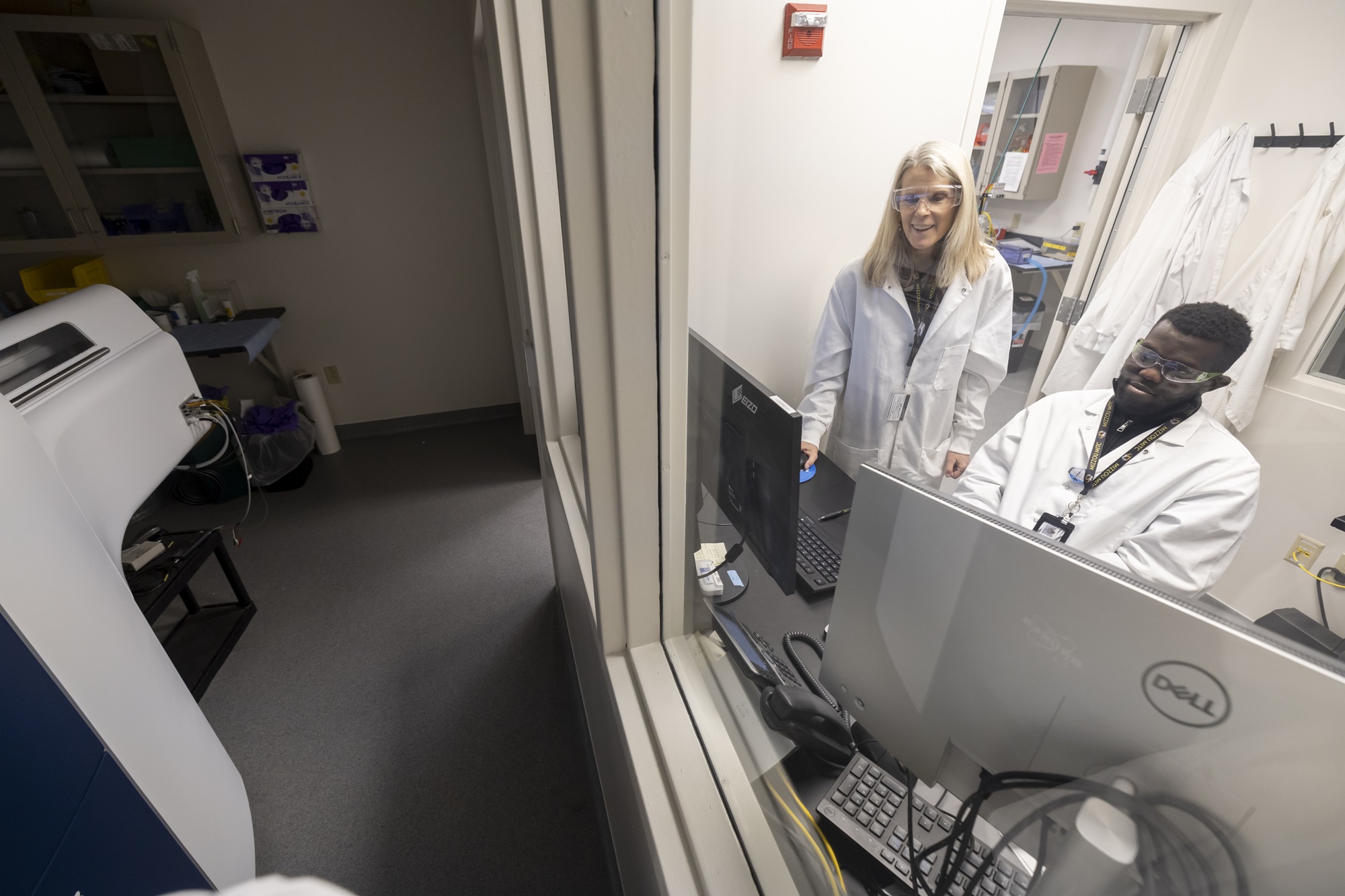
Anderson and her team are working to find the right targeting molecule for a radiopharmaceutical carrying terbium-161 to successfully bind with its target. As Hennkens produces small amounts of the radioisotope at MURR for her work, she shares some of that material with Anderson’s team to accomplish its task.
And what Anderson discovers can influence Hennkens’ future work.
“Dr. Hennkens’ group is pioneering new ways to produce isotopes, and her research will ultimately help bring terbium-161 into patients’ lives,” Anderson said. “My lab’s role is to test the terbium-161 with various types of cancer-targeting molecules and then feed that information back to the Hennkens’ lab for further optimization.”
Adding to the toolbox
Personalized medicine is an increasingly popular and innovative approach in health care that tailors medical care to the specific cancer an individual is battling. Radiopharmaceuticals represent just one of the many exciting aspects of the future of that approach.
While Anderson and Hennkens are respectively in the early stages of their research with terbium-161 at MU, Anderson is excited for the possibilities once Hennkens begins to scale-up her research using the reactor at MURR. At that point, Anderson’s team will begin conducting efficacy studies for terbium-161 in small animal models, which is the next step in the bench-to-bedside process.
Their end goal is to contribute to the development of a radiopharmaceutical with a targeted treatment method like Lutathera® or Pluvicto® that are approved for human use.
“Right now, this is one of the few places in the United States where we can do this type of research,” Anderson said. “With the resources at MU, including MURR, we are on the cutting edge of this research, and terbium-161 may be the next big radioisotope.”
This work was supported by the Department of Energy Office of Science (Office of Isotope Research and Development and Production). Funding was also provided in part by a National Institute of Health grant and from internal funds through the University of Missouri. MU has been a partner in the DOE IP University Isotope Network since 2017.