June 23, 2025
Contact: Janese Heavin, heavinj@missouri.edu
In a significant leap forward for successful cancer surgery, researchers at the University of Missouri and collaborators have developed a new imaging probe to help surgeons more accurately identify and remove aggressive tumors during operations.
The tool is expected to be a critical advancement in the fight against glioblastoma, one of the most difficult-to-treat brain cancers. In the future, it is intended to be expanded for image-guided surgery of various other solid tumors.
Described in a new study in Nature Publishing Group Imaging, the innovation works by pairing a fluorescent dye with a fatty acid molecule that cancer cells readily absorb. When introduced into the body, the compound is taken up by tumor cells, causing them to glow under near-infrared light, revealing cancer that might otherwise remain hidden.
Glioblastoma is considered surgically incurable because the tumor doesn’t stay in one place — it spreads and invades healthy brain tissue in a diffuse, microscopic way. This makes it impossible to remove completely without risking serious damage to brain function.
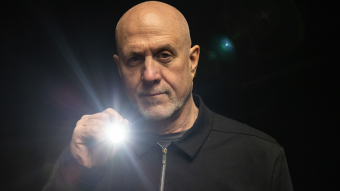
“Surgery remains one of the primary treatments for many cancers,” Elena Goun, associate professor of chemistry in the College of Arts and Science and one of the lead authors of the study, said. “In breast or prostate cancer, surgeons can often remove the tumor along with surrounding tissue. In brain cancer, that’s simply not possible. You must preserve healthy brain tissue. But if even a few cancer cells are left behind, the disease will return.”
That dilemma is especially acute with glioblastoma, which doesn’t form a neatly contained mass. Instead, it sends out microscopic extensions — finger-like projections that blend into healthy brain tissue and are invisible to the naked eye.
Because of this, surgeons must walk a fine line: removing as much tumor as possible while avoiding harm to vital brain areas. The more thoroughly the tumor is removed, the more effective follow-up treatments like radiation and chemotherapy tend to be.
The new small-molecule probe, known as FA-ICG, is engineered to solve that problem. It links a natural long-chain fatty acid (FA) to indocyanine green (ICG), an FDA-approved near-infrared dye widely used in surgical imaging. This fatty acid-based approach means the probe is highly selective: glioblastoma cells, which thrive on fatty acids, absorb it more than normal brain cells. That makes the cancer stand out more clearly.
The result is a tool that takes advantage of cancer’s altered metabolism to highlight tumor cells from within.
“Surgeons would view a monitor during surgery showing where the probe is lighting up,” Goun explained. “If they still see fluorescent signals, it means cancer is still present and more tissue needs to be removed. When the light disappears, they would know they’ve cleared the area.”
In the operating room, surgeons already use a variety of tools to guide tumor removal — including microscopes, ultrasound and fluorescent dyes. Of those, fluorescent dyes are particularly useful because they make otherwise invisible tumor cells light up under special lighting.
Right now, the only approved imaging dye for glioblastoma surgery is 5-ALA, which fluoresces under blue light. But 5-ALA comes with major limitations: The operating room must be darkened in order to see it, tissue penetration is shallow and the fluorescent signal is often weak and non-specific.
It also comes with side effects — most notably, photosensitivity, meaning patients must avoid bright light exposure after surgery due to the risk of skin and eye damage.
That’s where the FA-ICG probe shines — both literally and functionally.
Compared to 5-ALA, FA-ICG is brighter, works under normal surgical lighting, and offers real-time visualization under the microscope — no need to turn the lights off mid-surgery. This saves time and makes procedures more efficient. The signal-to-background ratio is also higher, meaning it’s easier to distinguish tumor tissue from healthy brain.
The FA-ICG probe is not only easier to see, it’s also easier to use. Its longer half-life allows more flexibility in scheduling surgeries, and the logistics of administration are simpler than with current probes.
“The upside of fluorescence-guided surgery is that you can make little remnants much more visible using the light emitting properties of these tumor cells when you give them a dye,” said Rutger Balvers, a neurosurgeon at Erasmus University Medical Center in the Netherlands, who is expected to lead human clinical trials of the probe. “And we think that the upside of FA-ICG compared to what we have now is that it’s more select in targeting tumor cells. The visual properties of the probe are better than what we’ve used before.”
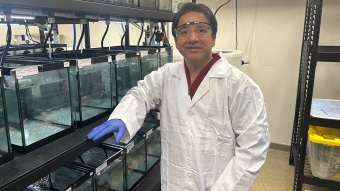
Michael Chicoine is a neurosurgeon at MU Health Care and chair of Mizzou’s School of Medicine’s Department of Neurosurgery. While he’s not directly involved in the research, Chicoine understands the potential benefits firsthand.
Currently, he said, MRIs are the gold standard for imaging tumors; however, they’re expensive and time-consuming, especially when required during an operation.
“This fluorescent metabolically linked tool gives you real-time imaging,” he said. “We could merge techniques, using the probe during surgery and saving the MRI for a sort of final exam. It’s definitely an exciting advancement.”
Researchers are also excited about other uses for the probe, including for other types of cancers and for use during follow-up treatments.
“After radiation or chemotherapy, it becomes very difficult to distinguish between scar tissue and active tumor,” Chicoine said. “This probe could give us a definitive answer — helping doctors know whether to continue treatment or adjust it, or consider another surgery. Eliminating the current uncertainty would be really helpful.”
Another promising use of the probe could be in photodynamic therapy either during or after surgery. Since the dye also has light-activated properties that can kill cancer cells, researchers are exploring whether it could double as a treatment tool, not just a diagnostic one.
Clinical trials for use in glioblastoma cases are expected to start in Europe, with strong interest already growing among neurosurgical teams.
The upcoming Phase 1 trial will focus on how patients tolerate the probe, whether there are any side effects at an effective dose and how its performance compares to existing tools. Ultimately, the goal is to make brain tumor surgery safer, helping surgeons remove all cancerous tissues while preserving as much healthy brain tissue as possible.
If results are positive, future studies could expand the use of FA-ICG beyond brain tumors to other cancers with high fatty acid metabolism, such as pancreatic cancer, fellow corresponding author Laura Mezzanotte from the Erasmus’ Department of Radiology and Nuclear Medicine said.
“Near-infrared fatty acid molecular probe for image-guided surgery of glioblastoma” was published in Nature Publishing Group Imaging.