Published on Show Me Mizzou April 27, 2023
Story by Dale Smith, BJ ’88
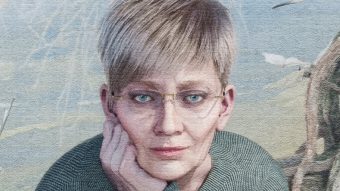
In Type 1 diabetes, or T1D, the body’s immune system goes rogue and kills the pancreas’s insulin-producing cells. For a century, the lifesaving treatment has meant enduring the multiple-times-daily jab — costly and painful injections of insulin that normalize blood sugar levels. Now, Haval Shirwan and colleagues have won a $3.2 million grant as they knock at the door of a groundbreaking new method of transplanting insulin-producing cells.
However, research is often a bumpy road, and their path is no exception.
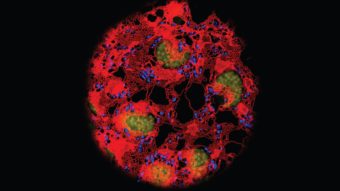
The team recently tested a promising method of transplanting pancreatic beta cells from donors. To their delight, insulin flowed in the preclinical studies. But two big barriers remained. The immune system recognized the transplants as outsiders and eventually destroyed them. Patients would have had to commit to a lifetime drug regimen shielding the transplant from bodily defenses. Those agents also lower resistance to a range of threats, including cancer. To boot, donor cells are too scarce to scale up this method.
Undaunted, the team sought out a new supply chain. They opened a collaboration with Washington University in St. Louis, where researcher Jeffrey Millman has figured out how to turn stem cells into a limitless supply of insulin-producing beta cells.
As for the immune system riddle, the team engineered a remarkable protein that, in a mere 10 minutes’ time, trains the immune system to accept the transplant as part of the body. Immune cells transform from attackers to allies that defend the transplant, which sits near the liver. This worked perfectly in early tests, which has caused quite a stir in the field.
The National Institutes of Health funding allows Shirwan and the team to combine the stem beta cells with the protein and examine the new transplant in preclinical trials.
Bumps may lie ahead, but, if the new process pans out as well in human patients, “It would be a game-changer, a cure,” Shirwan says. Patients with insulin-resistant T1D would be an early target for care. Children could be screened for genetic markers showing a predisposition to diabetes and receive preventive treatment. Beyond that, the approach could well adapt to many other autoimmune diseases such as lupus and multiple sclerosis.
To read more articles like this, become a Mizzou Alumni Association member and receive MIZZOU magazine in your mailbox. Click here to join.