Mizzou’s most ambitious collective scholarly initiative ever is set to merge innovation, technology and research to develop and deliver life-saving treatments to the public. Officials broke ground June 21 on the $220.8 million NextGen Precision Health Institute, a 265,000-square-foot research facility on the northwest corner of Hospital Drive and Virginia Avenue. A ribbon-cutting ceremony celebrating its completion is scheduled for Oct. 19, 2021. The event also launched the NextGen Precision Health Initiative, which harnesses and supports the University of Missouri System’s research activities and health system.
Top MU investigators will conduct research in the facility alongside other accomplished scientists to be recruited internationally. They will work in the areas of cancer, vascular disease and neurological disorders, including Alzheimer’s, PTSD, stroke and many other conditions. Construction funding will come from MU, the University of Missouri System, the state of Missouri, industry partners and private donors.
“The difference between the institute and any research facility we’ve built before is our intent to take the research to the people of Missouri and beyond,” says Mark McIntosh, UM System vice president of research and economic development. “As important as the basic research is, it comes down to our ability to translate that research into action in the community.”
The translational aspect of the facility is in keeping with Mizzou’s mission as a land-grant university. Whether it’s engaging the public in clinical studies, using videoconferencing to help patients in underserved communities or creating models for unlocking the mysteries of traumatic brain injury, the initiative’s overarching goal is to develop biomedical innovations that improve health.
“This will be a facility where we bring together the immense strengths of the MU campus and University of Missouri System,” says Elizabeth Loboa, dean of the College of Engineering and vice chancellor for strategic partnerships. One way of translating the strengths from “benchtop to bedside” will be through partnering with private companies. MU faculty and staff will work side by side with industrial scientists in the building’s innovation tower to identify and pursue discoveries with the best chance of improving lives.
To meet these goals, clinicians and researchers will be engaged in the second aspect of the institute, precision health. Rather than treating whole populations of people using the same approach, practitioners of precision health consider each person’s genetic makeup, lifestyle and environment during diagnosis and treatment.
Investigators create precision health treatments and cures in part by collecting and analyzing massive amounts of data from both animals and humans, says Loboa, whose College of Engineering includes a strength in big-data analytics. “For instance,” she says, “computer algorithms can optimize approaches to diagnose what disease a person might have.” MU already has a track record of developing such insights. Collaborative research among the School of Medicine, the College of Veterinary Medicine and the MU Research Reactor has led to medical breakthroughs for humans as well as companion animals. In addition, MU’s National Swine Resource and Research Center is the nation’s best at producing gene-edited pigs that serve as models for researchers working to cure disease. Occupational therapists in the School of Health Professions are using algorithms to personalize therapy for stroke patients by programming virtual reality video games to meet specific needs. Algorithms also play an important role at TigerPlace, a public-private partnership between Americare Systems Inc. and the Sinclair School of Nursing. Sensor technology developed at TigerPlace in collaboration with the College of Engineering brings precision health to senior care in the form of alerting nursing staff to potential health problems in time to prevent them.
The institute will enhance these types of collaborations by bringing scientists and other professionals together in one place, McIntosh says. “You put all these people in the same spaces and let them collide, and the more collisions you have, the more innovations you get.”
The institute will position the university as a global leader in cutting-edge science and biomedical research for the 21st century, says Chancellor Alexander N. Cartwright. “Generating that kind of impact for our communities, our state and the world is what Mizzou has always been about.”
Innovation at the intersections
Public-private partnerships will be baked into studies at the NextGen Precision Health Institute, where companies aligned with the research will work with faculty to identify the most promising technologies and help bring them to the marketplace.
“We want to be doing not just the best research in the world but also to have outcomes that improve health care and reduce costs for patients,” says Elizabeth Loboa, dean of the College of Engineering. To achieve these goals, the facility’s innovation tower will provide space where industry leaders work side by side with MU researchers.
“Sometimes in the academic space we’re focused on research we’re doing,” Loboa says. “We’re publishing papers, we’re educating our students, and that’s important. But the aspect of translating those technologies and getting them out into the marketplace — that’s also really important.” Such industry partnerships also shape the workforce by training students in innovative technologies and approaches.
“Innovation lies at the intersections,” Loboa says. “Our strengths lie in the differences we bring to the table.”
Gray matters
 As part of the neuroscience core at the institute, scientists will bring what’s been called an “invisible injury” into the open. Traumatic brain injury caused by concussive forces outside the body can disrupt brain function and pose a risk for PTSD as well as neurodegenerative diseases such as Alzheimer’s. With cases of traumatic brain injury on the rise in military populations, scientists at the Harry S. Truman Memorial Veterans’ Hospital are teaming up with MU and Missouri University of Science and Technology to create an Open Field Blast facility. “We’re developing this core facility as a national resource to look at war-like trauma conditions that impact our military personnel and veterans,” says Adam Whaley-Connell, associate chief of staff for research and development at the veterans’ hospital. The facility will simulate combat conditions in a controlled environment, creating a model for research on traumatic brain injury and other neurological diseases, he says.
As part of the neuroscience core at the institute, scientists will bring what’s been called an “invisible injury” into the open. Traumatic brain injury caused by concussive forces outside the body can disrupt brain function and pose a risk for PTSD as well as neurodegenerative diseases such as Alzheimer’s. With cases of traumatic brain injury on the rise in military populations, scientists at the Harry S. Truman Memorial Veterans’ Hospital are teaming up with MU and Missouri University of Science and Technology to create an Open Field Blast facility. “We’re developing this core facility as a national resource to look at war-like trauma conditions that impact our military personnel and veterans,” says Adam Whaley-Connell, associate chief of staff for research and development at the veterans’ hospital. The facility will simulate combat conditions in a controlled environment, creating a model for research on traumatic brain injury and other neurological diseases, he says.
Companions in health care
When Kay and Cottrell Fox took their 13-year-old dog to Mizzou’s Veterinary Health Center, they knew their English springer spaniel Molokai would take part in pioneering research. But they couldn’t have guessed where it would lead.
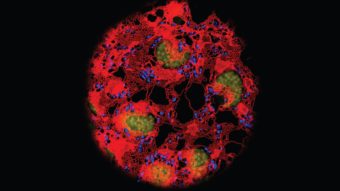
That was back in 1997, and Molokai was one of the first bone cancer patients that College of Veterinary Medicine clinicians treated with a form of targeted radiation called Quadramet®. The drug, which contains a radioactive ingredient from Mizzou’s research nuclear reactor, eased Molokai’s pain for the remainder of her life.
Ten years later, Kay’s father was treated for bone cancer. “I went over to hug him, and he said I needed to stay away from him for 24 hours,” she says. “It’s the same advice we got for Molokai.” Indeed, in the intervening decade, collaborative research between the veterinary college and the School of Medicine had made Quadramet® available to relieve bone cancer pain in humans, as well.
Mizzou is one of a handful of universities nationwide housing both disciplines on one campus — a constellation of talent and resources that brings together not only companion animal and medical research but also engineers, computer scientists and industry leaders to accelerate life-saving discoveries for animals and humans alike. MU’s strong track record in this “one-health” approach to research is set to leap forward with the institute as a new hub.
The Foxes have given the veterinary college an estate gift of more than $5 million in honor of their family veterinarians: James Schuessler, DVM ’82, and the late Fred Bendick, BS Ag ’68, DVM ’70. “These gifts will be put toward research that will benefit people and dogs and will advance our war on cancer,” says Jeffrey Bryan, who directs the college’s Comparative Radiobiology and Epigenetics Laboratory.

Video therapy
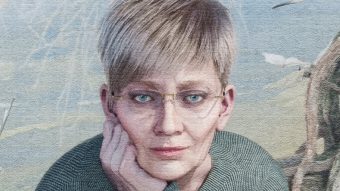
“Only perfect practice makes perfect,” the saying goes. But when it comes to recovering from a stroke, what’s perfect for each patient, and how does that target move over time? Cindy Downing (pictured below) found herself wondering about such questions five years ago while doing occupational therapy after a stroke. No stranger to hard work, Downing, co-owner of the Copper Kettle restaurant in Ashland, Missouri, followed through on her physical therapy. But when she learned about an MU study using video games to improve outcomes by fine-tuning therapies and increasing compliance, she gave the behavioral science approach a try.
Working with occupational therapy faculty member Rachel Proffitt, Downing played a game called Mystic Isle twice a day for 30 days. Proffitt incorporated into the game customized movements such as reaching forward and side to side as well as standing up out of a chair.
Downing’s stamina and range of motion improved dramatically. “Aside from a few fine motor skills, like flipping an egg, which are a work in progress, we’re getting there,” Downing says.
A Microsoft Kinect camera tracked Downing’s movements, allowing Proffitt to adjust the game’s intensity to challenge Downing but not overwhelm her. “It’s why people keep playing Candy Crush on their phones,” Profitt says. “It’s just the right level of challenge.”

Sharing knowledge and saving lives at a distance
Last winter, Karen Edison got the kind of news every academic physician wants to hear. Through her guidance, a health care provider picked up on a symptom of ovarian cancer in time to save a patient’s life. Edison, immediate past chair of dermatology and medical director of the Missouri Telehealth Network, had been advising the patient’s provider, a longtime participant in Show-Me ECHO (Extension for Community Healthcare Outcomes). ECHO is a relatively new type of knowledge-sharing resource that links health care providers throughout the state with a multidisciplinary team of medical experts via teleconferencing. Participants hear a short lecture followed by discussions on cases they’ve sent ahead of time. An outgrowth of telehealth, which involves working with one patient or provider at a time, Show-Me ECHO expands its reach to underserved areas by educating many providers at once, thus helping more patients. “About 60 melanomas have been diagnosed that wouldn’t have been because of dermatology ECHO,” Edison says. “We’re also doing ECHOs in autism, asthma, hepatitis C, chronic pain, opioid use disorder, child psychiatry, high-risk OB and more.”
Precision pigs
Anyone who tuned into The Daily Show back in March 2006 might have caught an MU curators’ distinguished professor describing some of his research. In a segment — “What are we doing to pigs?” — Randy Prather explained how scientists from MU and the University of Pittsburgh edited the genes of pigs to produce a healthier food source. Host Jon Stewart responded sarcastically: Rather than changing one’s diet, surely it would be easier to rearrange a pig’s cellular structure.
All joking aside, the study is just one example of how Prather and his research team are using genetically modified pigs to help diagnose and treat human and animal diseases. Prather directs MU’s National Swine Research and Resource Center, the only NIH-funded swine resource center in the country. “Nobody else has this set of techniques and expertise to be able to make these genetically modified pigs,” Prather says.
He and his team have made 75 models that could help researchers at the NextGen Precision Health Institute and elsewhere as they develop new treatments for a number of diseases and disorders, including cystic fibrosis, for which 1 in 25 North Americans is a carrier. “Cystic fibrosis is a big breakthrough,” Prather says. “Until we genetically modified the pigs to develop cystic fibrosis, there wasn’t any other organism besides
human children who had the symptoms of the disease.”
Physicians can monitor pig models as a disease progresses, and they can work to develop treatments and cures in a way they can’t with humans. Compared to other lab animals, pigs have cardiovascular and immune systems more like those of humans, Prather says. “If you want to study some of these diseases, there’s no other choice but pigs.”

A rare resource
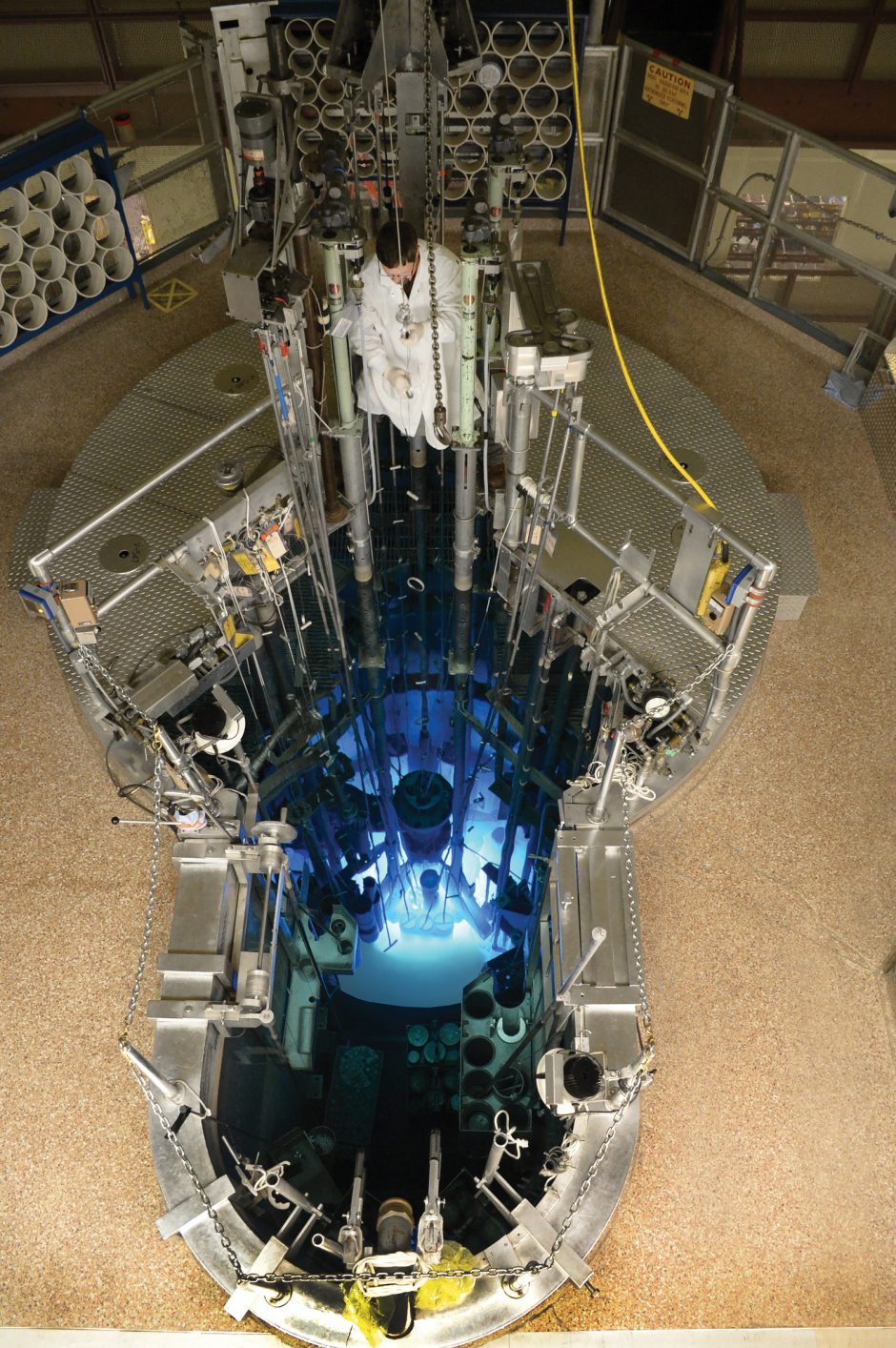
For more than 20 years, Nicole DiCamillo had endured a roller coaster of painful symptoms and discouraging prognoses with her life-threatening neuroendocrine tumors. Finally, in 2016, she started to get relief when doctors began treating her with a drug containing lutetium-177, which is made at the MU Research Reactor (MURR.)
“The treatment is a form of radiation, but it’s not like what we all remember,” DiCamillo says. “It’s so much better than earlier forms because it targets just the tumors and shrinks them.” A new approach to diagnosis and therapy called theranostics enables physicians to pinpoint DiCamillo’s tumors and treat them with precision.
David Robertson, director of research at MURR, likens theranostics to a taxicab that accepts only certain cargo — in this case, the isotope gallium-68, an imaging agent, and the radioisotope lutetium-177. The cab delivers gallium-68, and the element acts like a GPS, producing images of the tumors and marking their locations. With that roadmap in place, the taxi delivers the radioactive lutetium-177 directly to the tumors. “This is really important because neuroendocrine tumors spread all through the mid-gut,” Robertson says. The drug allows physicians to deal with each patient’s response individually, monitoring progress, or, if the treatment isn’t working, discontinuing the therapy.
MURR makes the majority of the world’s supply of lutetium-177 as well as other drugs for conditions such as inoperable liver cancer and pain from metastatic bone cancer. The reactor’s ability to supply radioactive isotopes for treatments that are less toxic and more efficient than traditional approaches makes it a rare and invaluable resource for creating new medical advances.
There are 25 research reactors in the U.S., but MURR is the largest by far. “We operate at 10 megawatts, providing the power to efficiently produce short-lived medical isotopes,” Robertson says. “We are the only reactor in the world that operates 52 weeks a year, ensuring a reliable supply of these critical isotopes that cannot be stockpiled.”
Custom senior care
How do you keep the elderly as independent as possible while reducing their risk of falls? It’s a common problem that challenged nurse-researchers at TigerPlace, a residential eldercare community in Columbia built through a public-private partnership between Americare Systems Inc. and the Sinclair School of Nursing (SSON).
Innovative solutions to the challenge emerged after Marilyn Rantz, executive director of the Aging in Place Project and Sinclair Home Care, approached the College of Engineering. Collaborative work between the SSON and Marge Skubic, director of the Center for Eldercare and Rehabilitation Technology, produced a noninvasive system of sensors that have revolutionized residential senior care.
Research has documented how these sensors alert the TigerPlace care team to signs of imminent falls, allowing time for early interventions. For example, depth sensors can capture changes in a resident’s gait three weeks before a fall is likely to happen. This allows staff to put physical therapy or environmental changes in place to improve function and help prevent the fall.
“Care at TigerPlace is customized for each resident,” says Kari Lane, TigerPlace operations director and an associate professor at SSON. “The sensors that we use at TigerPlace ‘learn’ the individual resident.” Rather than basing alerts on the general population, the sensors collect data from a resident and generate an alert when patterns change. The sensor technology, along with other components of precision health such as recognizing the importance of diet and lifestyle, contribute to the goal of keeping residents healthy and independent.
Studies have found that the use of sensors, combined with the registered nurse care coordination team at TigerPlace, allowed residents to stay in independent housing 2.5 years longer than without them. “We really work hard to keep people at TigerPlace through end-of-life and help them remain as independent and active as possible,” Rantz says.

To read more MIZZOU magazine stories online, visit mizzou.com.