
Cancer research doesn’t normally start this way.
Abe Eisenstark, research director for the Cancer Research Center in Columbia, studies salmonella. But not just any salmonella. Old salmonella. Salmonella strains he got from his mentor, Milislav Demerec, who got them from 1958 Nobel Prize– winner Joshua Lederberg, who got them from a Swedish scientist named Kaare Lilleengen, who pulled them from Swedish sewage in the 1940s.

In the 1950s and ’60s, Eisenstark and his geneticist colleagues vivisected the salmonella strains with bacteriophages, which are viruses that attack bacteria. They were learning the bacterium’s genetics and creating a taxonomy of the bacteriophages.
But eventually they packed the salmonella strains into nearly 3,000 neatly labeled inch-tall glass vials, sealed them in wax, and moved on to other projects. They stored the pertinent information for each vial in a catalog of IBM punch cards. For decades, the tubes sat on wooden shelves in a rear storage room at the MU-affiliated Cancer Research Center, a nondescript, single-story brick building on Columbia’s east side.
Then, one day in 2003, at Eisenstark’s direction, a scientist named Alison Dino grabbed a few of the samples. One by one, she popped their caps, dropped their contents into petri dishes and placed the dishes under an inverted tissue culture microscope in MU’s microscopy lab. Eisenstark had the wild notion that these tiny bacteria could be a new weapon in the fight against cancer.
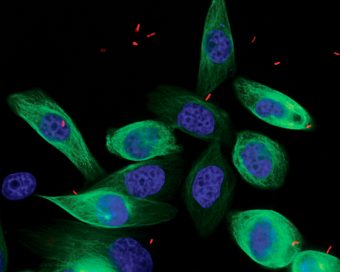
Peering into the microscope, Dino was looking for two things: whether the salmonella were drawn to tumor cells on one side of the petri dish and whether they shunned healthy cells on the other side. If they invaded the cancerous cells, that would be good. If they simultaneously left the healthy tissue alone, that would be perfect. Such behavior would be evidence that the bacterium causing one of the world’s most common food-borne illnesses could be a cure to one of the world’s most common deadly diseases — cancer.
Dino knew how “out there” the idea sounded. So, when she looked into the microscope, she couldn’t help herself. She started laughing.
Her boss’s wild idea was right.
Bacteria and Cancer: It’s Complicated
To be fair, the notion that salmonella could treat cancer wasn’t new in 2003.
Research as far back as the 1890s suggested that bacteria (streptococcus in that case) could shrink tumors. The problem lay in the poisonous side effects, which seemed unavoidable. For a century, it was a research dead-end.
Fast-forward to 2002. A research team from Yale University published a study on salmonella as a cancer-fighting agent in mice. As in the past, the bacterium showed promise, but a follow-up study in dogs was cut short when the treatment proved fatally toxic to one of the dogs.
Nevertheless, Eisenstark, a professor emeritus of biological sciences at MU, read the study with great excitement — or, rather, with greater excitement than usual. Eisenstark compares the joy of reading the latest scientific journals to the joy he felt reading the day’s newspaper comics as a kid. It’s the sort of enthusiasm that explains why he started his doctoral studies at the University of Illinois directly after returning from service in World War II, where he’d worked as a medic in the Pacific theater for the U.S. Army, diagnosing soldiers with malaria. He didn’t even go home first.
So, after reading the 2002 Yale paper, Eisenstark rushed off to New Haven, Connecticut, and spoke with the authors. He had big ideas for a follow-up study of his own, and the Yale researchers encouraged him to pursue it.
His idea built on the Yale findings, which were based on the central observation that viruses and bacteria often prefer to attack organisms at particular sites — a trait called cell selectivity. It’s why a cold virus makes you cough and sneeze but doesn’t give you diarrhea: It likes the respiratory system, not the digestive system. Similarly, salmonella is attracted to tumor cells. The bacterium is adept at penetrating the cell membrane, multiplying inside and destroying the tumor cells’ mitochondria — its power plant. The Yale research showeds almonella will pass 1,000 healthy cells to attack one cancerous one. However, it also releases toxins into the body. The Yale team had genetically manipulated its salmonella strain to make it less toxic, but they hadn’t made it safe enough.
That’s where Eisenstark thought his salmonella might have a leg up. He had a hunch that, after 50 years of mutating in confinement, at least one of the 3,000 strains in his storage closet would have lost its toxicity naturally.
The logic works like this: Imagine a family loses electrical power to their house. They have a backup generator, but that won’t last forever. They adapt by conserving power, shutting down nonessential appliances. No more big-screen. Goodbye, lava lamp.
Sticking bacteria in a small vial with a drop of food is akin to shutting off the electricity. Knowing that his salmonella had spent decades in that environment, Eisenstark predicted subsequent generations of salmonella would adapt by turning off nonessential functions, including toxin production. He calls it “natural tempering.”
Judging from the research done on similar long-lived salmonella strains, Dino had a good idea which of theirs might have tempered best. So when she did her petri dish test in 2003, she didn’t pop the caps of all 3,000 vials; she grabbed just a few of the most promising candidates. She had put only a couple vials under the microscope before she found the laugh-inducing CRC 1674.
The bacteria placed in the same petri dish as the cancerous tissue darted straight to the tumor cells, like a parched person seeking water. Yet, the bacteria placed with the healthy tissue showed no interest. They turned their metaphorical thirsty heads away, demanding bottled water, not tap. Critically, the bacteria also produced toxins at much lower levels than any strain scientists had studied previously.
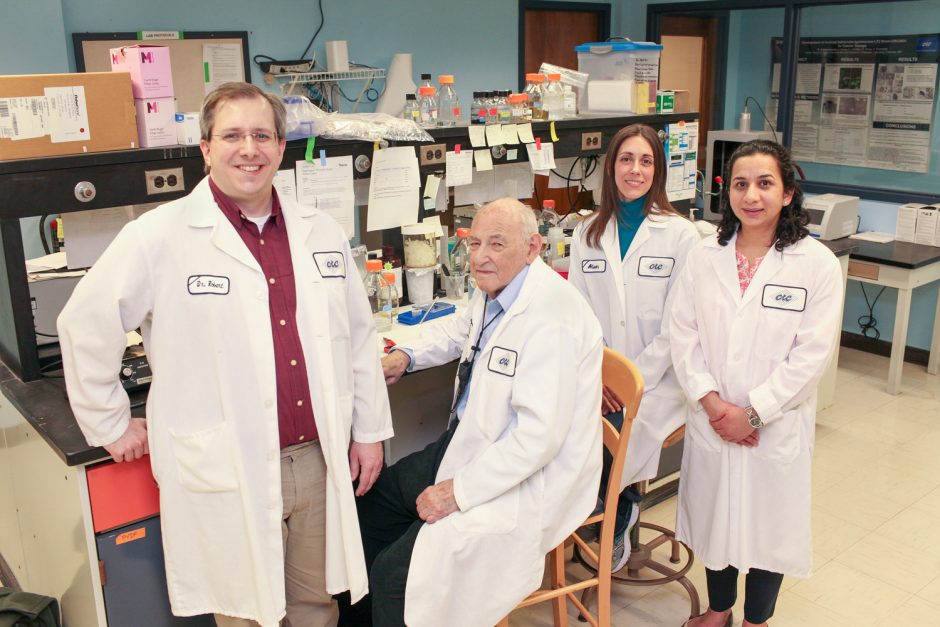
They knew they were on to something. The next step was to call Robert Kazmierczak.
Detox

Kazmierczak, the Cancer Research Center’s research senior investigator, specializes in genetic manipulation. His job was to remove every shred of toxicity he could find in CRC 1674.
Although genetic manipulation gets quicker and easier all the time, it still takes years. By 2006, Kazmierczak had made enough changes to CRC 1674 that he designated it as a new strain, CRC 2631. The new version is even less toxic to healthy cells than the original and more disruptive to cancer cells.
But Kazmierczak isn’t done yet. He designed a scaffold for the strain, to which researchers can attach cancer-fighting agents. Think of it as a roof rack for a car — you can attach luggage, skis, kayaks, or, in this case, cancer-fighting proteins. He is also designing a version of CRC 2631 that would use the bacterium’s own genes to produce cancer-fighting agents from within the tumor cells.
Such abilities could be key to CRC 2631’s success. The first study of the strain in mice, published in 2016, used animals prone to prostate cancer. The salmonella was able to target the tumors, replicate and live inside them, and even shrink their size. But it was unable to stop their spread.
While the scaffolding work continues, the Cancer Research Center team, which includes research fellow Bakul Dhagat Mehta, will test the strain in a larger mammal to assess its safety and effectiveness.
They are working with Jeffrey Bryan, MS ’04, PhD ’07, associate professor of medical oncology at MU’s College of Veterinary Medicine, toward a clinical trial of dogs with leukemia, to begin as early as 2018.
Having Bryan nearby as a collaborator is a godsend for the team. “It speeds us along a lot,” Kazmierczak says. “It would cost a fortune to pay someone to design that experiment.”
Developing a cancer treatment out of salmonella fits the current trend in immunotherapy, Bryan says. Researchers are taking advantage of the cell selectivity of bacteria and other organisms to deliver treatments directly to disease sites. This approach avoids the side effects of traditional cancer treatments that inject chemotherapy into the bloodstream, where it flows throughout the body to healthy and cancerous tissue alike.
Penn State is working on a similar treatment for osteosarcoma cancer in dogs using the listeria bacterium. “You’re seeing this pop up all over the place,” Bryan says.
His leukemia study will use dogs whose owners choose experimental treatment at the MU Veterinary Hospital.
Canine versions of human chemotherapies cost thousands of dollars, are much more likely to be toxic to our four-legged friends and are less effective. They only hold the cancer at bay, Bryan says. They don’t cure it. If the CRC 2631 strain proves safe and effective in dogs, the research center team will seek approval for human trials from the U.S. Food and Drug Administration.
The Long Game
Science marches fast only in retrospect. The day-in, day-out slog of testing hypotheses — and finding the money to pay for those tests — takes time. Progress accrues over years, even decades.
Eisenstark is well acquainted with the long view on this point. He started his research program in 1948, when he took his first faculty job at Oklahoma State University. He came to Mizzou in 1970 to lead the Division of Biological Sciences. But his ambition for microbiology goes back to his boyhood, when he became enamored of the image of scientist-heroes fighting disease. He loved the 1936 film The Story of Louis Pasteur and kept a tattered copy of Sinclair Lewis’s novel Arrowsmith long into his professional career.
So, when he sealed up the 3,000 salmonella strains decades ago, he did so knowing that they were worth keeping, hoping that they would play a part in a scientific breakthrough.
Given that time scale, the 15 years since the Yale study prompted this new research have flown by. For a man who still finds joy in his work, he couldn’t have asked for more.
“I’m really pleased,” Eisenstark says. “I’m having a great time.”
Correction: A previous version of this story incorrectly identified the name of the Sinclair Lewis novel.



