Feb. 5, 2020
Contact: Brian Consiglio, 573-882-9144, consigliob@missouri.edu
Nerve damage that leads to a loss of feeling or numbness in the feet is a big problem for the millions of Americans living with diabetes. As a result, foot ulcers can go untreated leading to infections and even amputations. Now, researchers at the University of Missouri are developing a bandage with “smart” capabilities that could help people with diabetes better treat foot ulcers so they can heal, improving their quality of life.
“The sensor-integrated bandages will send data to both the patient and clinician’s cell phone to provide feedback on how much pressure is being applied to the affected foot,” said Xueju “Sophie” Wang, assistant professor of mechanical and aerospace engineering in the MU College of Engineering. “Similar to a stoplight, a green signal will indicate the wound is healing, a yellow signal will indicate more off-loading is needed, and a red signal will indicate far too much pressure is being applied.”

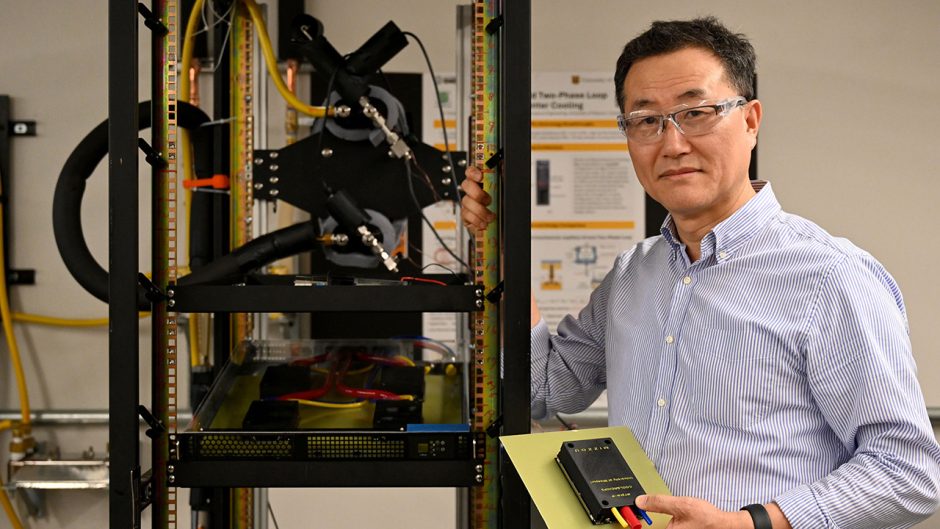
Carolyn Crumley and Xueju "Sophie" Wang collaborated to develop a sensor-integrated bandage that can help improve healing rates for people with diabetic foot ulcers.
Wang is joined by Carolyn Crumley, an adjunct assistant professor in the MU Sinclair School of Nursing. As a practicing nurse at St. Luke’s East Hospital near Kansas City, Crumley works with many patients with diabetic foot ulcers who have used various boots and shoes that are specially designed for off-loading, or minimizing the weight applied to the affected foot. However, she has found that patient compliance can be difficult due to the bulky and uncomfortable equipment. Wang, whose research interests include high performance battery materials, is collaborating with Crumley to develop a system that can be easily integrated with bandages to track patient compliance in a quantitative way.
“Patients love receiving feedback, and we hope this product will help them start to see the direct correlation between keeping pressure off the wound and the wound healing,” Crumley said. “This is a great way to improve collaboration between the health care provider and the patient so that they are both on the same page throughout the recovery process.”
The researchers recently received a grant from the MU Coulter Biomedical Accelerator Program to develop their smart bandage, the program’s first grant awarded to the Sinclair School of Nursing. The MU Coulter Program bridges the gap between academic research and industry by providing funding to help engineer-clinician teams turn their ideas into products.
“The Coulter Program provides training, funding and other resources to innovators like Drs. Crumley and Wang,” said Jaya Ghosh, program director of the MU Coulter Biomedical Accelerator. “Their research highlights the power of interdisciplinary collaboration; we are proud to help them take their innovation from lab to market where it can positively impact patient care.”
Crumley expects the smart bandages to improve healing rates and ultimately the quality of life for people with diabetic foot ulcers. She said Wang and herself have already heard some positive responses from industry leaders interested in potentially partnering with the team to take the product to market.
“From finding business partners to filing patents, the Coulter Biomedical Accelerator Program has provided us with mentorship in addition to the grant funding,” Crumley said. “It is rewarding to see the impact that multidisciplinary research can have on helping people with diabetes.”