Contact: Brian Consiglio, 573-882-9144, consigliob@missouri.edu

Throughout her 38-year nursing career, Laurel Despins has progressed from a bedside nurse to a clinical nurse specialist and has worked in medical, surgical and cardiac intensive care units. She noticed diabetes is rarely referred to as a primary cause of death in itself, yet the disease is a leading contributor to deaths involving heart disease, stroke and cancer.
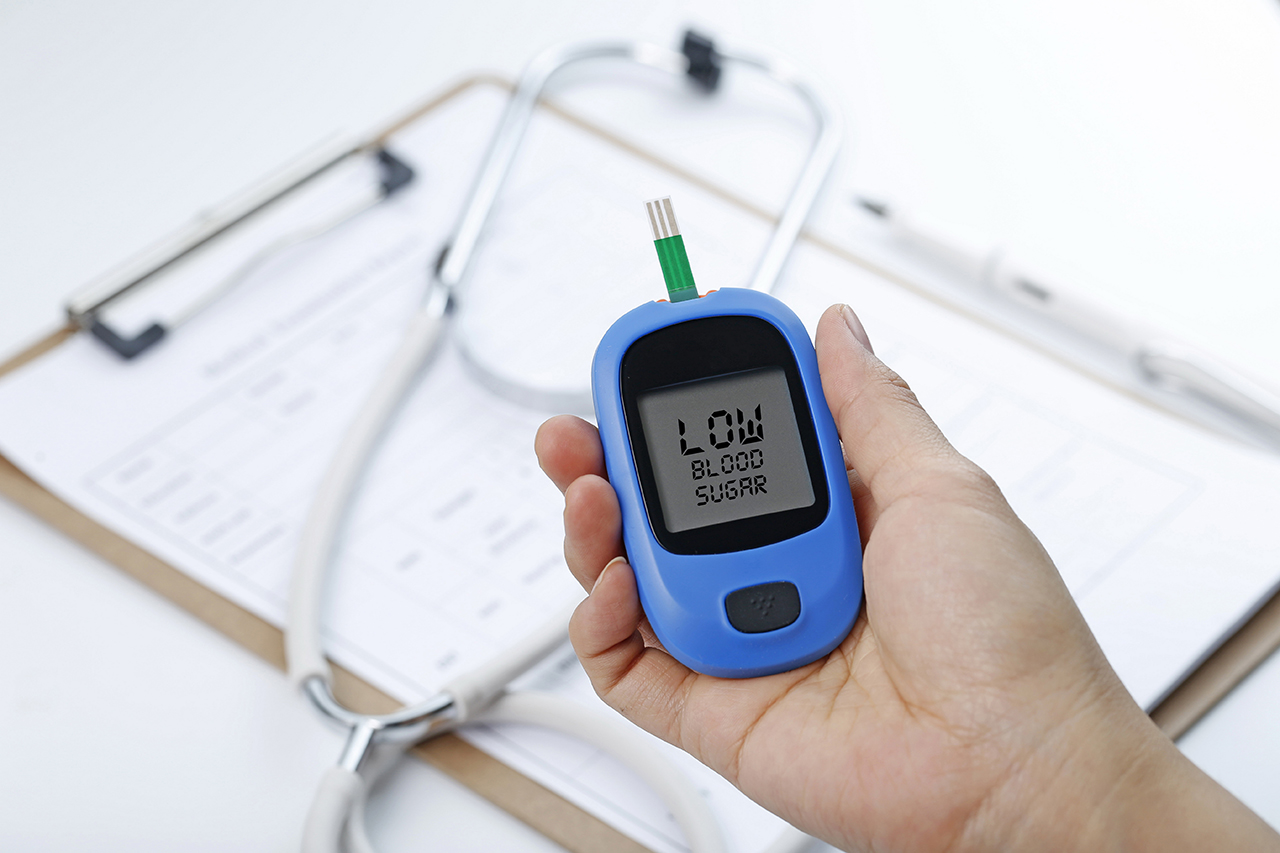
“In addition to being a contributor to cardiovascular-related deaths, diabetes can lead to a variety of negative health outcomes, such as kidney failure, arthritis, nerve issues, eye problems and leg ulcers that can become infected,” said Despins, now an assistant professor and researcher in the MU Sinclair School of Nursing. “Therefore, creating a plan to keep blood glucose levels from getting too high or too low will help those with diabetes better manage the disease and avoid those negative health complications down the road.”
To help adults with diabetes better manage their blood sugar levels, Despins interviewed individuals diagnosed with type 2 diabetes about their understanding of the disease and their approach toward self-management. She found those who had previous life experiences watching a relative or neighbor manage diabetes influenced how they viewed diabetes management themselves.
“For example, one subject grew up watching his grandma inject insulin needles into her thigh all the time like it was no big deal, so naturally that person did not look at diabetes as something to be overly concerned about,” Despins said. “On the other hand, another subject saw his neighbor with diabetic leg ulcers and swore that he never wanted that to happen to him, so he was very attentive to monitoring his blood sugar levels.”
Because there is no one-size-fits-all approach to diabetes management, Despins says healthcare providers need to better understand the life circumstances of their diabetic patients, including their financial resources.
“People on a fixed income might not be able to routinely buy fresh produce instead of pasta, which can impact their blood glucose levels,” Despins said. “Given the tough circumstances some people with diabetes live in, health care providers need to do an assessment of what resources patients with diabetes have available so they optimize what they can do.”
To better serve patients with diabetes, Despins recommends that when health care providers collect initial quantitative data from patients such as weight, height and age, they should also ask additional qualitative questions to get a better understanding of the patients’ knowledge of the disease.
“Asking questions like ‘What do you currently know about diabetes?’, ‘Do you know someone with diabetes?’ and ‘How do you think they did at self-managing it, and does this influence the way you view your self-management plan?’ will help the health care provider better understand the patient’s life experiences,” Despins said. “My overall goal is to help people with diabetes better optimize their self-management, which will improve their health outcomes by avoiding negative complications in the long run.”
“Making sense of blood glucose data and self-management in individuals with type 2 diabetes mellitus: A qualitative study” was recently published in the Journal of Clinical Nursing. This project was supported by grant number R24HS022140 from the Agency for Healthcare Research and Quality. The content is solely the responsibility of the authors and does not necessarily represent the official views of the Agency for Healthcare Research and Quality.