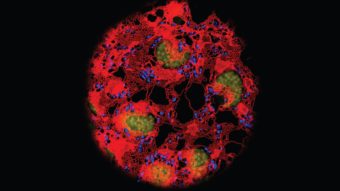
When MU physicians prescribe opioid painkillers, they receive an automated alert if the patient in question is at high risk for abuse. When doctors order a blood transfusion for patients whose hemoglobin level is above the minimum threshold of 7 grams per deciliter of blood, they are reminded that the transfusion might not be necessary. And when a combination of vital signs shows a patient is deteriorating — and possibly in the early stages of the deadly infectious disease sepsis — a signal summons a nurse immediately and ensures a physician will get to the bedside within 15 minutes.
All these alerts, known in health care lingo as “clinical decision support systems,” are triggered by algorithms written into the electronic health record, or EHR. But the EHR is not just a digital version of the old paper chart physicians dictated and typists tapped out for each patient. It is a technological tool that makes care safer, more efficient and less expensive. And it provides an enormous vein of data for medical researchers.
“There are a lot of bees buzzing around that record,” says pediatrician Tom Selva, chief medical information officer for MU Health Care. “Not all of them are doing the same thing at the same time, but they allow you to have a disinterested machine sitting in the back looking at all the data and maybe seeing the patterns we don’t see. That’s cool stuff.”
The authors of those algorithms — the beekeepers who make the cool stuff possible — are members of the Tiger Institute for Health Innovation. The institute is the IT department born a decade ago from a partnership between the University of Missouri and Cerner Corp., the Kansas City-based health care IT company. Ten years into the relationship, the institute has helped transform Mizzou into a national leader in technological innovation.
Unleashing an IT Tiger
In the fall of 2009, former University of Missouri System President Gary Forsee and former Cerner CEO Neal Patterson agreed to what was then a unique arrangement. Rather than perpetuating a traditional vendor-client relationship, they created the institute, a Columbia branch of Cerner devoted to using technology to improve the health of Missourians.
“When you have a vendor as your IT company, you call them when you have a problem,” says Stevan Whitt, a critical care physician and chief medical officer of MU Health Care. “It’s you giving them work to do. A lot of times, they charge you for it, so it’s not like they’re unwilling to do it, but they don’t have the same time and quality imperatives that you do. But Tiger Institute works on-site and is part of the university. When we call them with a problem, it’s not my problem, it’s our problem.”
When health care providers spot issues such as opioid addiction, unnecessary blood transfusions or sepsis, they lead a team that investigates ways of dealing with the problem. Each project team includes at least one institute staffer who can customize Cerner algorithms, and the new technology has legs. For example, when Cerner observes high blood transfusion rates at another hospital, it recommends the program designed at MU.
When the institute was created, hospitals nationwide were scrambling to comply with the federal HITECH Act, which promised financial incentives to providers that switched from paper patient records to EHRs and met the government’s “meaningful use” standards. Rather than sitting in one filing cabinet, an electronic record is more easily accessible wherever patients seek treatment in a health system. That gives providers instant information about a patient’s medical history and helps them make efficient, informed decisions.
After digitizing MU’s hospitals and clinics, the institute expanded the EHR to include neighboring hospitals in Osage Beach and Jefferson City. So, if a patient sees a primary care physician near the Lake of the Ozarks and a specialist in Columbia, the providers can coordinate care. Patients in any of the three health systems can use HEALTHConnect, an app the institute developed that lets patients schedule appointments, view their records and renew prescriptions on their phone or computer. More than 100,000 patients have such accounts.
Since achieving the meaningful use standard in 2014, the push has been toward improving outcomes.

The Results
The institute, which has more than 180 employees and interns, has helped Mizzou earn national recognition for its use of technology from the Healthcare Information and Management Systems Society (HIMSS). In 2012, MU Health Care received the highest grade — Stage 7 — for its inpatient facilities, which placed it among the top 1.9 percent of all U.S. hospitals. The next year, it reached Stage 7 for its ambulatory clinics. In 2015, HIMSS bestowed upon MU its highest honor, the Davies Award of Excellence.
“When we won the Davies Award, we had to demonstrate to auditors that we had saved $60 million,” Selva says. “Yes, we saved $60 million getting rid of medical records rooms, repurposing the staff, paper we weren’t using and patient mishaps that weren’t occurring.”
And the clinical decision supports are paying off, as well.
In the fight against sepsis, the Tiger Institute customized an algorithm that alerts doctors and nurses based on the National Early Warning Score. The NEWS system assigns points to a patient’s vital signs and compiles a score — the higher the score, the sicker the patient. During a three-month pilot phase of implementing NEWS in University Hospital’s medical specialties unit, the mortality rate dropped from 3.4 percent to 2.5 percent, which translates to eight lives saved. The notification is now in place throughout the hospital.
The opioid alert reminds doctors who are writing prescriptions that high-risk patients need to sign an opioid treatment agreement. The document is scanned into the EHR and lets other doctors know they shouldn’t prescribe painkillers to the patient. The alert also suggests which patients should be prescribed the opioid rescue drug naloxone so loved ones can administer it in case of an overdose. During the alert system’s first two months in use, doctors accessed opioid treatment agreements four times more often than before and wrote more than twice as many prescriptions for naloxone as they did previously.
In the blood management alert system’s first year, MU Health Care reduced the number of transfusions by 13 percent, saved $195,000 in blood acquisition costs and avoided spending up to $1.14 million in indirect costs associated with transfusions.
“It is rare to visit an institution like ours where the CEO will tell you, ‘One of the foundations of our success is our IT department,’ ” Selva says. “But that’s true here because they are us. It’s a partnership. Health care is really about ingesting information and making decisions and sharing information. Well, health IT and health care have become a very blurred line when all the technology is brought to bear.”
To read more articles like this, become a Mizzou Alumni Association member and receive MIZZOU magazine in your mailbox. Click here to join.